1120 NW 14th Street / Miami, FL 33136
Lumbar Fusion in 2025: How New Technology Is Changing Spine Surgery
Dr. Shelby Burks
Lower back pain is one of those things people try to live with for a long time. They stretch. They rest. They push through workdays. They tell themselves it’ll calm down. For some patients, it doesn’t. When pain starts affecting walking, sleep, or basic movement — and conservative treatments stop helping — lumbar fusion may enter the discussion. That word alone can feel intimidating. What many patients don’t realize is how much lumbar fusion has changed in recent years. Especially heading into 2025.What Lumbar Fusion Is Meant to Do
At its core, lumbar fusion is about stability. It’s used when movement between spinal segments causes pain or nerve compression. Common reasons include:- Degenerative disc disease
- Spinal instability
- Spondylolisthesis
- Severe arthritis
- Certain disc or nerve conditions
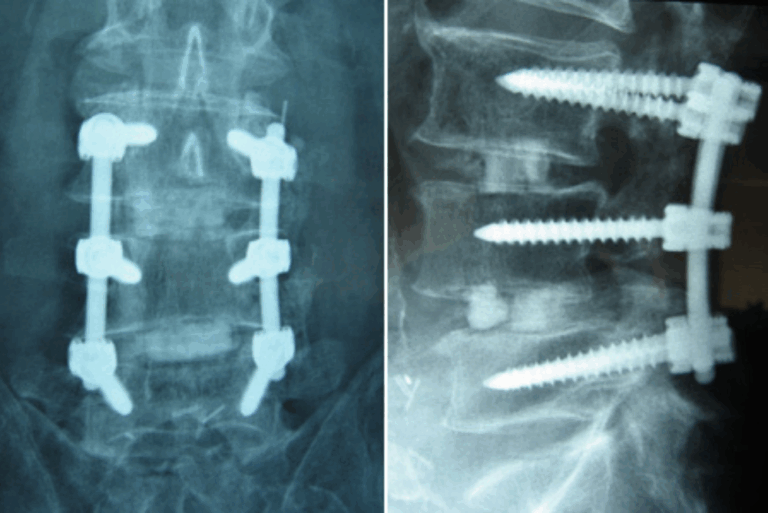
What’s Actually New About Lumbar Fusion Today
Lumbar fusion used to mean larger incisions, longer hospital stays, and slower recovery. In 2025, the approach looks very different. Newer technology allows for:- Smaller, more precise incisions
- Better visualization of spinal anatomy
- More accurate implant placement
- Less disruption to surrounding muscle
- More predictable alignment
Minimally Invasive Techniques Matter More Than Ever
One of the biggest shifts has been how fusion is performed. Minimally invasive lumbar fusion techniques aim to:- Preserve muscle instead of cutting through it
- Reduce blood loss
- Decrease post-operative pain
- Allow earlier movement after surgery
- Shorter hospital stays
- Quicker return to daily activities
- Less post-surgical stiffness
Navigation and Imaging Improvements
Technology now helps surgeons see more — and plan better. Advanced imaging and navigation systems allow for:- More precise screw placement
- Better spinal alignment
- Reduced reliance on guesswork
- Improved consistency from case to case
Modern Implants and Materials
Fusion hardware has evolved as well. Today’s implants are designed to:- Match patient anatomy more closely
- Support proper spinal alignment
- Encourage better bone healing
- Reduce implant-related complications
What Recovery Looks Like Now
Recovery after lumbar fusion is still a process — but it’s more manageable than it used to be. Most patients notice:- Leg pain improves before back stiffness
- Movement becomes easier gradually
- Strength returns over time
- Walking
- Avoiding heavy lifting
- Protecting the surgical area
- Gradual return to activity
Risks Haven’t Disappeared — But They’re Better Managed
No spine surgery is risk-free. Potential risks include:- Infection
- Bleeding
- Nerve irritation
- Hardware issues
- Non-fusion (rare, but possible)
Is Lumbar Fusion Always the Right Answer?
No. And that’s important. Some patients do better with:- Physical therapy
- Injections
- Activity modification
- Non-fusion surgical options
Dr. Shelby Burks’ Approach
Dr. Shelby Burks focuses on using technology when it adds value, not just because it exists. That means:- Careful diagnosis before surgery
- Matching technique to anatomy
- Using minimally invasive options when appropriate
- Prioritizing long-term function, not just short-term relief
What a Consultation Typically Involves
Patients usually go through:- Review of imaging (MRI, CT, X-rays)
- Discussion of symptoms and daily limitations
- Explanation of surgical and non-surgical options
- Honest discussion of recovery and risks
- Clear expectations moving forward

