1120 NW 14th Street / Miami, FL 33136
How Is a Laminectomy Performed in 2025?
A Clear, Modern Explanation from Dr. Shelby Burks
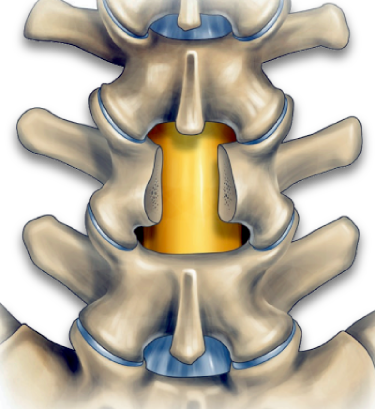
Most people don’t come in asking for spine surgery. They come in because something isn’t working anymore — pain that won’t settle down, numbness in the legs, weakness, or the feeling that standing or walking is becoming harder every month. For some patients, that leads to a conversation about a procedure called a laminectomy. The word alone sounds intimidating. But the surgery itself has changed a lot — especially in the last decade. Here’s how a laminectomy is actually performed in 2025, what’s different now, and how surgeons like Shelby Burks approach it today.What a Laminectomy Is — In Plain Terms
A laminectomy is a procedure designed to relieve pressure on the spinal cord or nerves. The “lamina” is a small piece of bone that forms the back wall of the spinal canal. When that space becomes too tight — often from arthritis, disc degeneration, or thickened ligaments — nerves can get compressed. That compression is what causes:- Back or neck pain
- Pain shooting into the arms or legs
- Numbness or tingling
- Weakness
- Difficulty walking or standing
What’s Different About Laminectomy in 2025
This isn’t the wide-open spine surgery many people imagine. Modern laminectomy is:- More precise
- More targeted
- Less disruptive to surrounding tissue
How Dr. Burks Performs a Modern Laminectomy
While every case is different, the general process looks like this: First, the surgery is planned using high-resolution MRI and imaging. This matters. The decision about how much bone to remove is made before the patient ever enters the operating room. During surgery:- A small incision is made over the affected spinal level
- Muscles are gently separated rather than aggressively cut
- Specialized instruments are used to remove the lamina causing compression
- Nerves are decompressed under direct visualization
- Stability of the spine is carefully preserved
Why Precision Matters So Much
Removing too little doesn’t help. Removing too much can cause problems later. This is where surgeon experience matters. Dr. Burks focuses on:- Preserving natural spinal structures
- Avoiding unnecessary fusion when possible
- Reducing post-operative stiffness
- Allowing patients to return to movement safely
What Recovery Typically Looks Like
Recovery is usually more manageable than patients expect. Most people experience:- Early relief of leg or arm symptoms
- Gradual improvement in strength and sensation
- Soreness at the incision site, not deep nerve pain
- Go home the same day or next day
- Walk shortly after surgery
- Return to light activity within weeks
When a Laminectomy Makes Sense — And When It Doesn’t
Not all back pain requires surgery. A laminectomy is usually considered when:- Symptoms persist despite conservative care
- Imaging shows clear nerve compression
- Pain or weakness is affecting daily life
- Walking distance or balance is declining
- Isolated muscle pain
- Mild, self-limiting back discomfort
- Imaging findings without symptoms
Why Patients Choose Dr. Burks for Spine Surgery
Patients often come to Dr. Burks after being told surgery is their only option — or that fusion is inevitable. What they often appreciate is:- A measured, anatomy-driven approach
- Clear explanations without pressure
- Surgical plans based on stability, not routine
- Experience treating complex spine conditions

