1120 NW 14th Street / Miami, FL 33136
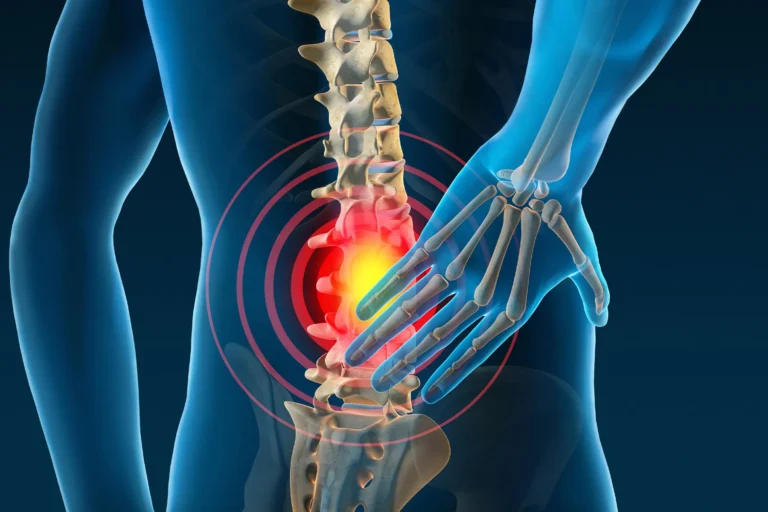
When Back Pain Is Not a Muscle Problem
A Patient-Focused Explanation Featuring Dr. Shelby Burks
Back pain gets blamed on muscles almost by default. A bad workout. Poor posture. Sleeping wrong. And sometimes, that’s true. Muscle strains are common and usually improve with rest, stretching, or time. But Dr. Shelby Burks sees many patients whose pain doesn’t fit that pattern at all. They’ve tried physical therapy. They’ve taken anti-inflammatories. They’ve waited it out. And the pain keeps coming back — or worse, it starts changing. Shooting down the leg. Burning. Numbness. Weakness. Pain that doesn’t care if you rest. That’s usually the moment when Dr. Burks starts thinking: this isn’t a muscle problem anymore.Why Muscle Pain Usually Improves — and Structural Pain Doesn’t
True muscle pain tends to behave in predictable ways. It flares after activity. It improves with rest. It gets better over days or weeks. Structural spine problems don’t follow those rules. Dr. Burks explains to patients that pain coming from the spine itself — discs, nerves, joints, or the spinal canal — often has a different “personality.” It may worsen with sitting. It may improve when leaning forward. It may wake you up at night. Or it may slowly steal strength without much warning. Those patterns matter more than the pain level alone.Common Non-Muscle Causes Dr. Burks Looks For
When patients come in convinced they “just pulled something,” Dr. Burks takes a step back and looks at the bigger picture. Some of the most common non-muscle causes include: Herniated or bulging discs These can irritate or compress nerves, causing pain that radiates into the arms or legs. Spinal stenosis A narrowing of the spinal canal that can lead to leg pain, heaviness, or weakness, especially with walking. Facet joint arthritis Pain coming from the joints of the spine itself, often worse with extension or rotation. Nerve compression Pain described as electric, burning, or sharp — often accompanied by numbness or tingling. Instability or degenerative changes Segments of the spine that move when they shouldn’t, leading to chronic pain and inflammation. Dr. Burks doesn’t assume one of these is present — he looks for clues in the history, exam, and imaging before drawing conclusions.Red Flags That Suggest It’s Not Muscular
One of Dr. Burks’ biggest roles is helping patients recognize when it’s time to stop guessing. Back pain is less likely to be muscular when you notice things like:- Pain traveling down the arm or leg
- Numbness or tingling
- Weakness or foot drop
- Pain that worsens with sitting or standing still
- Pain that improves only in certain positions
- Symptoms lasting longer than 6–8 weeks
- Night pain or pain at rest
Why Imaging Alone Isn’t the Answer
Many patients arrive with an MRI report already in hand. Dr. Burks reviews imaging carefully — but he’s quick to explain that pictures don’t equal diagnosis. Plenty of people have disc bulges with no pain at all. Others have severe symptoms with minimal findings. What matters most is how imaging matches:- Your symptoms
- Your neurologic exam
- Your daily function
Conservative vs Surgical Care — It’s Not One or the Other
A key reason patients trust Dr. Burks is that he doesn’t jump straight to surgery — and he doesn’t dismiss it when it’s clearly needed. When pain isn’t muscular, treatment may still start conservatively:- Targeted physical therapy
- Medications
- Injections
- Activity modification
- Nerves are at risk
- Function is declining
- Pain is persistent despite appropriate care
- Structural problems clearly explain symptoms
Why Patients Seek Dr. Burks Specifically
Patients often come to Dr. Burks after being told:- “Your MRI isn’t that bad” — despite worsening symptoms
- “It’s just muscular” — months later
- “You’ll always have pain” — without explanation

